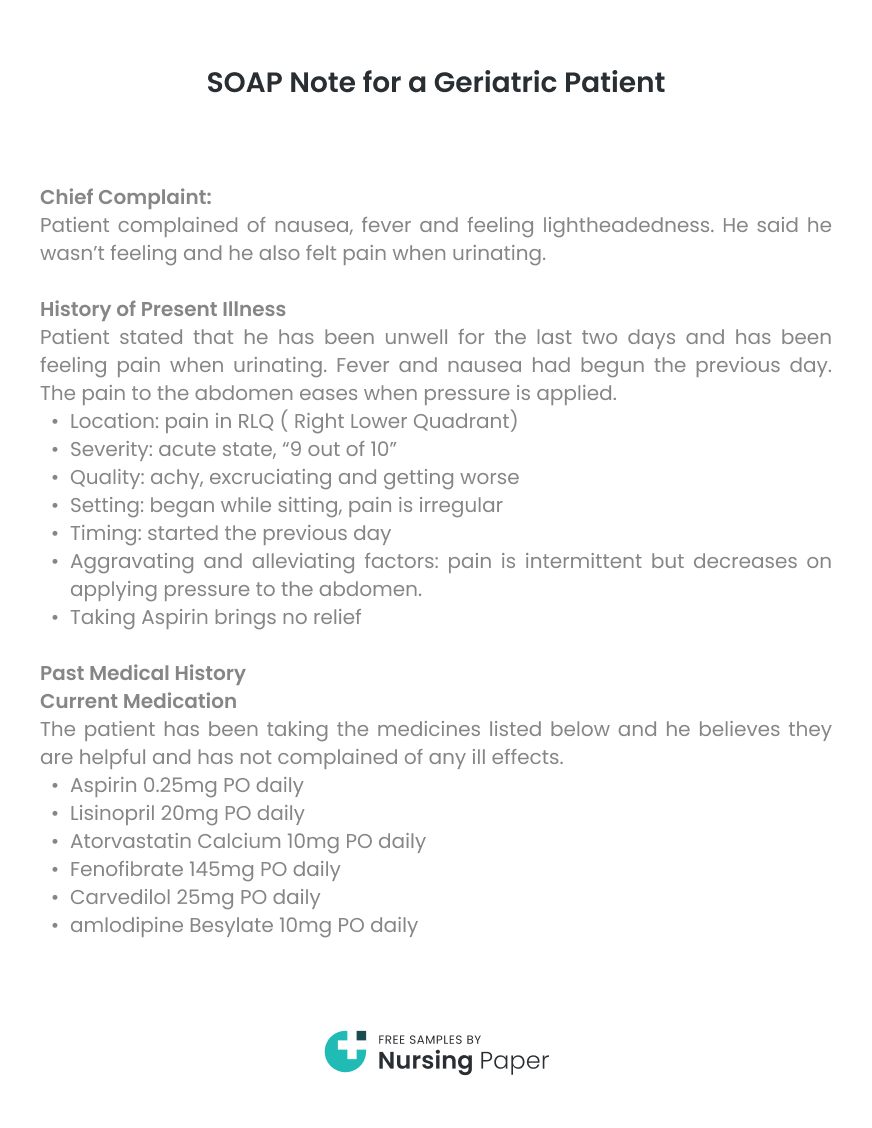
SOAP Note for a Geriatric Patient
Chief Complaint
Patient complained of nausea, fever and feeling lightheadedness. He said he wasn’t feeling and he also felt pain when urinating.
History of Present Illness
Patient stated that he has been unwell for the last two days and has been feeling pain when urinating. Fever and nausea had begun the previous day. The pain to the abdomen eases when pressure is applied.


- Location: pain in RLQ ( Right Lower Quadrant)
- Severity: acute state, “9 out of 10”
- Quality: achy, excruciating and getting worse
- Setting: began while sitting, pain is irregular
- Timing: started the previous day
- Aggravating and alleviating factors: pain is intermittent but decreases on applying pressure to the abdomen
- Taking Aspirin brings no relief
Past Medical History
Current Medication
The patient has been taking the medicines listed below and he believes they are helpful and has not complained of any ill effects.
- Aspirin 0.25mg PO daily
- Lisinopril 20mg PO daily
- Atorvastatin Calcium 10mg PO daily
- Fenofibrate 145mg PO daily
- Carvedilol 25mg PO daily
- amlodipine Besylate 10mg PO daily
Allergies: Latex

BEER’s Criteria: The medicines being taken are fine and there is no need to prescribe alternative drugs
Current Health Status: Overall, the patient is looking okay.
- Prior illnesses: Patients has in the past suffered from kidney disease and heart disease.
- Immunization status: Patient receives Shingles and Pneumococcal Vaccines annually.
Family History:



- Patient denies any family history of asthma, glaucoma, TB, diabetes, pulmonary disease, urological problems, HIV/AIDs, family violence, epilepsy, mental retardation, congenital abnormalities or psychiatric illness
Social History:
- Marital status: Widow
- Occupation: retired teacher
- Education: college
- Habits: does not drink or smoke
- Lifestyle: lives alone but family visits
- Resources: Medicaid
Systems Review
- Constitutional symptoms: Pain when urinating, fever, nausea and Light headedness
- Eyes: Patient wears glasses but presently he does not feel any pain.
- Nose: Has a good sense of smell and there is no pain
- Ears: Can hear well and there is no pain
- Mouth: He uses dentures and he cleans them dally. No pain is being felt
- Throat: There is no hoarseness or pain
Objective Data
Constitutional symptoms:
- Patient is alert and there is no acute distress. He appears a little unwell but is well hydrated. The behavior and speech appear normal.
- Temp: 101 Pressure: 134/70 sitting Pulse 97 BMI 28.9%
Eyes: No lesions can be seen and the conjunctiva is clear.
Ears: There are no lesions or masses.
Nose: No deformity noted and the mucosa is pink
Throat: Thyroid is normal and no masses are noted. The mucous membranes are moist and pink. The throat is pink and patient wears dentures.
Cardiovascular: Pulse rate: 97. The rhythm is regular. No indication of peripheral edema and the neck is supple.
Respiratory: Respiration rate: 16. Clear breathing sounds and no distress or wheezing noted.
General Inspection: Bowel sounds are normal and there is no evidence of hernia. There is tenderness in Right Lower Quadrant.
Musculoskeletal: No pain, masses or swelling noted.
Lymphatic: No acute bleeding or swelling noted. No bruising or trauma to the skin.
Psych: No assessment done because the patient was in pain
Neuro: There are no visible tremors or weakness. The patient has a normal gait.
Diagnostic Testing:
- UA (Urinalysis) – Moderate amounts of blood present,
- CBC (complete blood count) with Diff – Elevated WBC (white blood cells)
- CRP (C-reactive protein) – revealed elevation (6.7)
- CMP (comprehensive metabolic pane) – Elevated Glucose, Decrease Na (Sodium)
- X-ray of Abdomen– Positive for kidney stones
- CT – Scan of abdomen– Bilateral non-obstructing Nephrolithiasis.
- PSA (Prostate specific antigen) – 58
Assessment
Differential Diagnosis
- Kidney Stones – This is due to patient experiencing intermittent pain and the location of the pain. He also has fever and there is no rebound tenderness upon palpation. This is one of the signs of kidney stones (Kogan, 2017). The CBC results indicate there is an infection while the CRP results also indicate an inflammation in the body (Fernandez, 2013). The X-ray rules that the kidneys are infecte
- Prostatitis – This due to the pain location, light headedness and fever. Painful or difficulty in urination is a sign of Prostatitis (Pathy, 2012). The CBC results indicate there is an infection while the CRP results show an inflammatory response.
- Nephrolithiasis – this is due to the results from CBC, CRP and CT scan. CT Scans are essential in ensuring that the pain being felt is due to kidney problem and not the appendicitis (Gallo, 2013).
Plan
The patient was counseled regarding the medications to take, limitations of activities to undertake and the disease process.
The patient was sent to the laboratory and X-ray room. Lab results indicate elevated CMP, CRP and WBC. The CT scan and X-ray reveal kidney stones are present. The results were communicated to the patient.
Patient to be given fluids and to take Motrin tablets for fever.
Medication Prescribed: Cipro 500 mg for Prostatitis to be taken for 10 days. PCP to be given later if needed.
Indication: It is used to treat bacterial infections mostly associated with Prostatitis.
MOA: it works by inhibiting enzymes that are necessary for bacteria to replicate DNA.
Follow – up: Patient to see urologist the next day. Patient to continue on Cipro medication and have PSA checked after two months.
Care Plan
Help the patient manage medication delivery, personal care responsibilities and other general mental, physical and social issues. Advise the patient on getting an aide if the family is not available.
Anticipate changes in the living environment that arise due illness and therefore ensure that the patients safety and health is guaranteed. All geriatrics needs is a little attention and it is important that this is provided for. If the family cannot offer the required level of attention then have the patient moved to a nursing home or any other suitable environment.
Ensure that there is continuous monitoring and reassessment. The family should ensure that they receive periodic update of how their elderly patient is doing and take necessary action if necessary to ensure continued health of the patient.
Caregivers Support
Advise caregivers to take necessary measures to prepare themselves adequately to carry out their roles and also give counsel on how to avoid caregiver burnout. Measures to be taken include attending to their own needs, asking for help when necessary and joining support groups.
Reflections
The elderly often suffer from numerous pains that they do not understand. It is critical that when observing and evaluating the elderly care is taken to ensure that the precise location of the pain is pinpointed. This will require the physician to do thorough tests to ensure the correct diagnosis is made. Evaluation of this patient was highly dependent on their judgment i.e. how they were feeling, their past history etc which is not very reliable. To improve assessment of patients, collaborating with other professionals is essential. For instance, in the above case, early collaboration with the urologist would have ensured that the patient is fully treated on the same day and therefore avoid making a second trip.
1. Fernandez, H. (2013). Fundamentals of Geriatric Medicine: A Case-Based Approach. New York, NY: Springer Science & Business Media, 342.
2. Gallo. (2013). Handbook of Geriatric Assessment. New York, NY: Jones & Bartlett Learning 54-55.
3. Kogan, M. (2017). Integrative Geriatric Medicine. New York, NY: Oxford University Press 87.
4. Leutenberg, E. R. (2016). The Complete Caregiver Support Guide: A Reproducible Workbook for Groups and Individuals. New York, NY: Whole Person Associates 102- 103.
5. Pathy, M. J. (2012). Principles and Practice of Geriatric Medicine. new York, NY: John Wiley & Sons, 45-47.



The download will start shortly.

The download will start shortly.
 Subject:
Medicine
Subject:
Medicine  Number of pages: 13
Number of pages: 13  Subject:
Nursing
Subject:
Nursing  Number of pages: 2
Number of pages: 2  Subject:
Medicine
Subject:
Medicine  Number of pages: 3
Number of pages: 3  Subject:
Medicine
Subject:
Medicine  Number of pages: 2
Number of pages: 2  Subject:
Medicine
Subject:
Medicine  Number of pages: 2
Number of pages: 2  Subject:
Medicine
Subject:
Medicine  Number of pages: 3
Number of pages: 3  Subject:
Health and Social Care
Subject:
Health and Social Care  Number of pages: 4
Number of pages: 4  Subject:
Health and Social Care
Subject:
Health and Social Care  Number of pages: 3
Number of pages: 3  Subject:
Health and Social Care
Subject:
Health and Social Care  Number of pages: 2
Number of pages: 2  Subject:
Nursing
Subject:
Nursing  Number of pages: 2
Number of pages: 2  Subject:
Nursing
Subject:
Nursing  Number of pages: 1520
Number of pages: 1520  Subject:
Health and Social Care
Subject:
Health and Social Care  Number of pages: 2
Number of pages: 2  Subject:
Nursing
Subject:
Nursing  Number of pages: 2
Number of pages: 2  Subject:
Nursing
Subject:
Nursing  Number of pages: 3
Number of pages: 3  Subject:
Nursing
Subject:
Nursing  Number of pages: 3
Number of pages: 3 
