Asking What Is Evidence-Based Practice in Nursing? Answered Here!
The consideration of current scientific evidence and practices is extremely important in order to gradually improve nursing care. Such an approach, also known as Evidence Based Nursing (EBN), is gaining more and more attention in nursing practice. Read on to learn about what is evidence-based practice in nursing, and discover the basic steps to your evidence based practice.
First of all, let’s formulate the basic evidence based practice definition before proceeding with the steps.
Evidence-Based Nursing (EBN) is a structured approach to delivering high-quality nursing care by combining:
- The nurse’s clinical expertise
- The most up-to-date, relevant research evidence
- The patient’s values, needs, and preferences
EBN is grounded in Evidence-Based Practice (EBP), which promotes modern, research-validated care methods to improve outcomes and guide cost-effective, safe clinical decisions.
Current EBP standards (AACN Essentials 2024–2025) now emphasize equity, digital health literacy, AI-supported decision tools, and patient-centered communication as integral components of evidence-based nursing.
The approach is based on evidence based practice (EBP). So why is evidence based practice important? EBN uses the most modern care methods and steps. These methods have been proven by evaluating high-quality studies and statistically significant research results. EBN’s goal is to improve health and safety while taking steps to provide cost-effective care to improve outcomes for both the patient and the healthcare system practices based on evidence. Take steps to learn more about the steps of evidence based practice here.
Reasons Why is Evidence Based Practice Important Explained
EBP allows taking steps for health professionals to draw conclusions about the evaluation of existing practices and standard operating procedures for clinical care from the practice. There is also much other reliable data available to address the problems they encounter daily.
Thus, EBP requires the use of the most current and up-to-date evidence based information and observations to take steps to solve clinical cases during practice. EBP helps to get rid of the outdated method of sole reliance on book knowledge. Medical professionals tend to base on it because they handle a lot of information for their evidence based practice essays, most of which they take from books.
Evidence-based practice should never be a rigid rulebook. Instead, it must combine:
- Results from high-quality studies
- A nurse’s professional judgment
- The patient’s preferences and lived experience
Only when these elements are aligned can EBP deliver the best possible outcomes.
Many institutions now require EBP competency for clinical advancement, as it improves safety scores, reduces readmissions, and supports value-based care initiatives.
According to experts, only when all steps of evidence based practice come together, can one achieve the best result and thus the best quality of care.
Take 7 Steps of Evidence Based Practice to Succeed
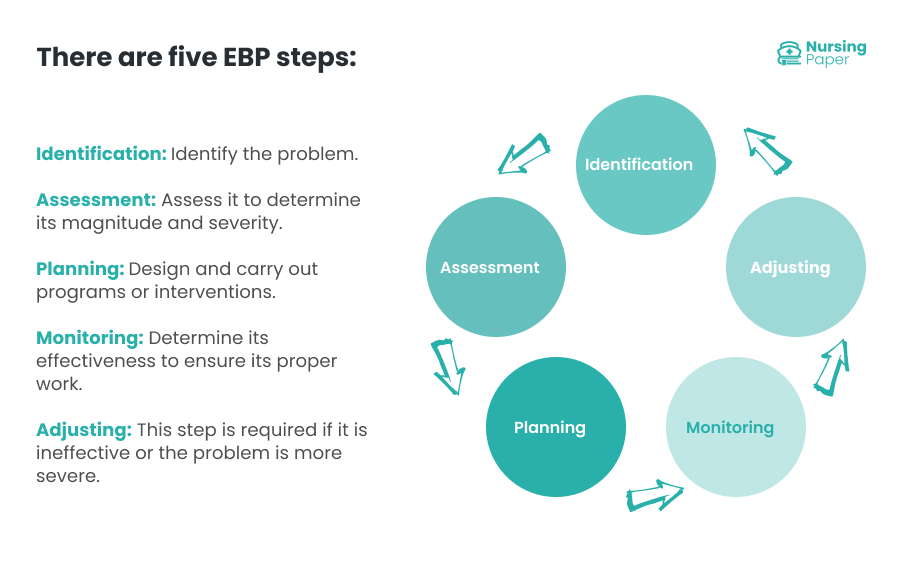
EBP is a process based on collecting, evaluating & integrating valid, clinically meaningful and applicable research. The evidence used to change practice or make a clinical decision can be divided into 7 steps of evidence based practice. They vary in research type and quality. For example, when searching for what is evidence based practice in nursing you’ll find that many proficient experts like ours often answer that there are just 5 basic steps.
1st step of evidence based practice: cultivating the Spirit of Inquiry. It’s the first among numerous steps of evidence based practice. An inquiring mind is an attitude that encourages one to ask questions about existing practices. Cultivating a spirit of inquiry allows health care providers to question current methods of practice. What’s more, it allows challenging those practices to bring about improvement and change. These are some key elements and steps to promote EBP:
- Always question current practices as a nursing professional.
- Incorporate EBP as a higher standard base and integrate competencies for EBP.
- Involve EBP mentors so skills and knowledge can be provided to others.
- Use tools to enhance EBP (e.g., meetings, educational/teaching time, access to, etc.)
- Increase support and the ability for leaders to model valued EBP skills.
Nurse leaders now use digital dashboards and AI-powered research search tools to help teams identify practice gaps and clinical improvement opportunities.
2nd Step: Formulating a PICOT Question
PICOT stands for:
- P – Patient, Population, or Problem
- I – Intervention
- C – Comparison
- O – Outcome
- T – Time frame
A well-constructed PICOT question guides an efficient, targeted literature search.
Asking questions creates a search that provides the most relevant and highest quality information on a topic. At the same time, this step reduces the time required to create those search results.
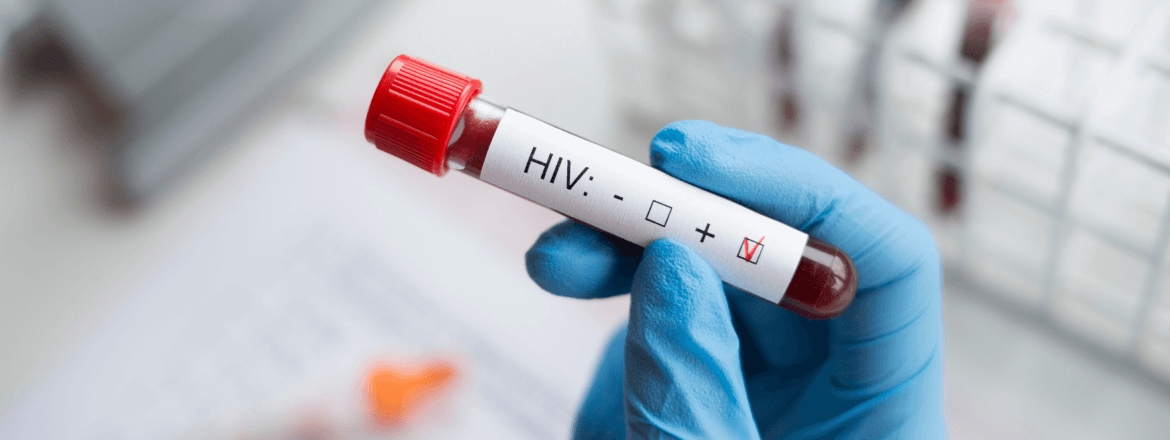
3d step of evidence based practice: searching for and collecting relevant evidence. To proceed with the steps of evidence based practice, you need to begin the search for evidence and use each keyword from the PICOT question you formed. Once you reach the decision on the intervention or treatment, you can assess the research to determine the strongest evidence. There are seven levels of evidence, with Level I being the strongest quality and Level VII being the poorest quality.
Modern EBP platforms now integrate machine-learning tools that help streamline literature searching and rank evidence based on relevancy and study quality.
4th step of evidence based practice: critically appraising the evidence. To begin the process of critical appraisal, you must ask three questions. It’s meant to determine the relevance of the evidence and whether it applies to the population served. The three questions from this step are:
- Are the research findings reliable?
- What are the outcomes?
- Are the results applicable to patient care?
After these three questions are asked, the evidence assessment continues by creating an evidence synthesis. This synthesis compares multiple studies to see if they are consistent with each other.
Updated appraisal tools (like the 2025 JBI and CASP revisions) now include guidance on evaluating AI-generated research and digital-intervention studies.
5th step of evidence based practice: integrating the evidence. After assessing the evidence, it must be linked to the provider’s expertise and the patient’s preferences. Medical professionals encourage patients to participate in decision-making processes. Therefore, the patient may decline treatment even if the trial is successful. In addition, examination findings and medical history may reveal further contraindications to a particular evidence based treatment. Finally, the availability of health resources may limit the implementation of treatment, even if it has been found to be effective in a trial.
Shared-decision frameworks, trauma-informed communication, and culturally responsive care are now considered essential components of evidence integration.
6th step of evidence based practice: evaluating results. The next phase is the steps of evidence based practice in nursing. The process is to evaluate whether the treatment was effective in terms of patient outcomes. Again, at this step, evaluating results to determine the impact of evidence based change on health care quality is important.
Assess whether the evidence-based change improved patient outcomes, quality of care, safety, and patient satisfaction.
Outcome metrics may include:
- Readmission rates
- Pain scores
- Medication adherence
- Patient-reported experience measures
Hospitals increasingly use real-time dashboards, EHR analytics, and digital tracking tools to measure clinical outcomes more accurately.
7th step of evidence based practice: disseminating results. The final step is to share the information, especially when positive results are achieved. By sharing the results of an evidence based practice nursing process, others can benefit. At this step, some methods for disseminating the information include presentations at conferences, roundtables within one’s institution, and journal publications.
Many institutions now require uploading EBP project summaries into internal digital repositories so teams across departments can replicate successful interventions.
Most Interesting Evidence Based Practice Nursing Topics to Choose
EBP nursing topics can cover a vast range of various areas. Sometimes, the choice of the appropriate topic might be a daunting task. At this step, whenever you are working on an EBP project, the easiest way would be to formulate it as a PICOT question. For example:
- The main aspects of care of intoxicated patients within the first 24 hours of hospitalization.
- The effects of insomnia treatment on hospitalized persons.
- Methods and techniques for communicating with those having depression.
- The methods for identifying psychosis-prone people.
- The best techniques for the care of those with suicidal tendencies.
Top trending EBP topics for 2025 include:
- Reducing nurse burnout with digital workload tools
- Improving patient outcomes using telehealth monitoring
- AI-driven fall-risk prediction models
- Post-COVID respiratory rehabilitation strategies
Equity-focused care models for underserved populations
Of course, these are just general ideas of your project’s topic we’ve gained from examples of nursing evidence based practice essays. However, you can use them as the basis for your own ideas and specific evidence based practice nursing topics ideas.
To integrate EBN into nursing practice, nurses must be aware of how important research is in terms of improving nursing care and the main steps of the process. The experiences of the nursing staff and the wishes of the patients should not take a back seat. The right steps are just as important as the study results. The aim of all steps should be to achieve a good mix and thus combine evidence and experience. The basic steps of evidence based practice in nursing allow medical professionals to achieve the best results in patient care.
EBP is now considered a core competency for all levels of nursing, from pre-licensure students to doctoral leaders, making it one of the most important skillsets in modern healthcare.